On Wednesday 22 September, 76 attendees joined an event on NHS Digital’s work on the Covid-19 situation.
Three teams from NHS Digital spoke about the analytical work they were involved in to support the response to the Covid-19 pandemic. Teams worked closely with partners in a range of organisations, including the University of Oxford, the Department of Health and Social Care, and the office of the Chief Medical Officer.
The projects discussed used bespoke data collections with routine and administrative data from multiple sources, and were subject to public and professional scrutiny. Links to each of the projects are available below.
Chief statistician Chris Roebuck kicked us off with an introduction to and summary of NHS Digital’s role generally and specifically in relation to the Covid situation.
Mental Health Survey of Children and Young People
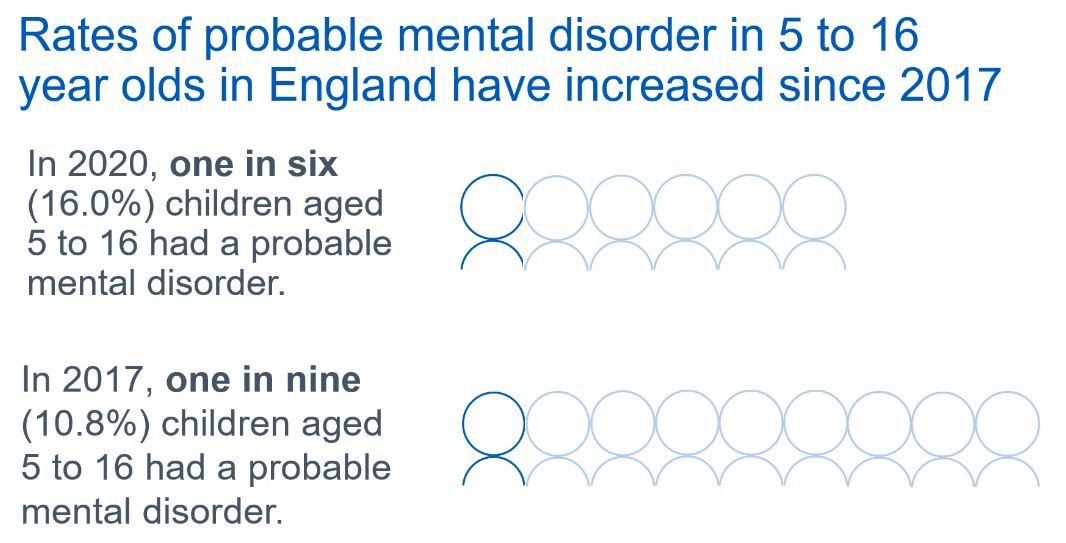
Sharon Thandi began our series of presentations with a discussion about a follow-up survey on mental health that started in 2017. The aims of the 2020 research were a) to compare the mental health of surveyed participants from 2017 and 2020, and b) to describe the life of participants during July 2020, in the midst of the pandemic. Sharon noted that the findings are estimates rather a descriptive summary statistics.
The work was only possible due to a large collaboration including The Department for Health and Social Care, the Office for National Statistics, Natcen and academics. The main survey tool used was the Strengths and Difficulties Questionnaire (SDQ), which classifies respondents based on the estimated likelihood of a having mental health disorder. Results showed a rise of estimated likelihood of a mental health disorder from 1-in-9 to 1-in-6.
Sharon shared many other findings that you can review on our live twitter stream of the session. Highlights in include gender differences and a possible relationship with measures of family functioning.
Funding has been acquired to conduct a further follow up study in 2022. Future reports will also include positive reflections on the effect of lockdown, recognising that mental health is not a negative concept.
Read the project report.
Risk Stratification and the NHS Digital ‘Shielded Patient List’
Our second speakers were Kieran Baker and Lucy Elliss-Brookes who talking spoke about Risk Stratification and the NHS Digital ‘Shielded Patient List’. Again, collaboration was key. NHS Digital worked with clinical colleagues to translate clinical concepts into technical specifications and rule sets to identify patients.
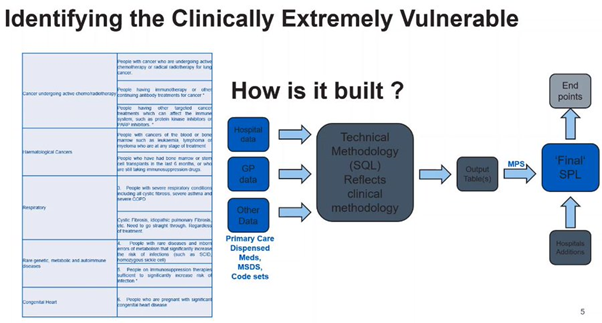
This required the development of bespoke data flows and databases in little over a week. This pressure was in addition to inevitable data quality issues, which included clinical codes disappearing from patients’ electronic health records, mistaken clinical codes - e.g. sickle cell trait vs sickle cell disease – and clarifying deceased status (which we learned can be formal or informal). You can peruse some of the details of the datasets on online dashboards.
Lucy Ellis-Brookes then spoke about subsequent work to host a risk-scoring algorithm for COVID outcomes, specifically QCovid. Data protection - privacy and security - were central to the implementation. This made it difficult to implement the risk-scoring algorithm because it required patient-level data. NHS Digital undertook deep critical reflection about the default imputations suggested by the original team in Oxford University.
The presentation was followed by a discussion about the consequences of the imputing missing values for risk scores. Following up with 1.5 million patients made individual augmentation to difficult. Inclusion or exclusion from the list was handled via subsequent communication with GP whom forwarded issues raised by patients.
Read the project report.
Covid in Primary Care publication
Our third talk was delivered by Rupert Chaplin and Efrosini about collecting Covid-related data from primary care. This augmented the usual primary-care record to facilitate analyses never possible before. Rupert made a point of noting that analyses were restricted to NHS England patients with a valid NHS number.
Efrosini presented on some descriptive analyses that used the COVID-augmented data. Interactive graphics are available for users to explore the analyses. As an example, comparisons were made between cases of COVID based on official statistics collected historically and those derived from the new, augmented, primary-care dataset.
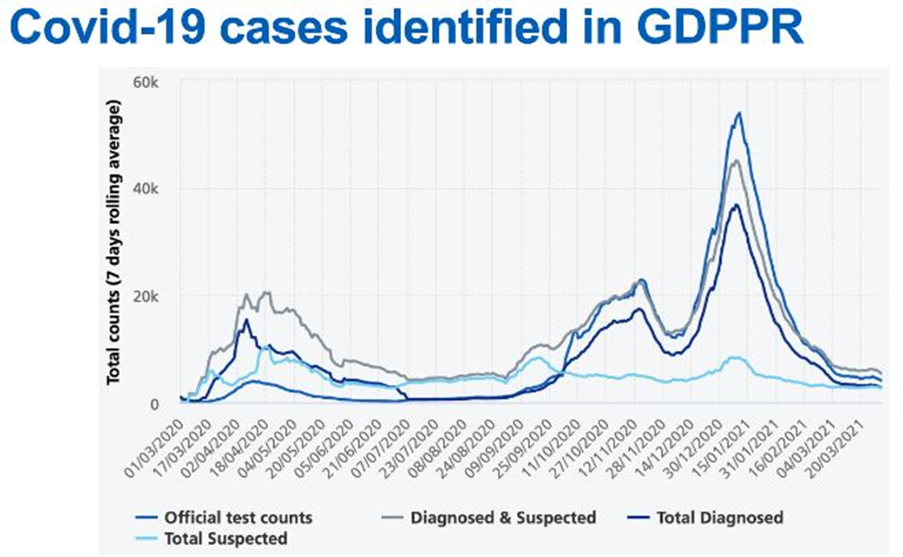
Comparisons were also made across ethic groups. Trends were similar across all ethnicities but magnitudes differed. It is important to note that the data only capture information about those that attended their primary-care practice. Rupert and Efrosini extended an invitation for inquiries: just email enquiries@nhsdigital.nhs.uk with 'Coronarvirus as recorded in primary care' in the subject line.
Read the project report.
We are very grateful to the speakers for their talks and for the audience’s engagement. You can review the twitter stream that was running alongside the event on our Twitter account, and a recording of the talk is available on the Leeds-Bradford local group YouTube playlist.
Author
Ciarán McInerney, PhD, is secretary of the Leeds-Bradford local group. He is a research fellow in the School of Computing at University of Leeds and the NIHR Yorkshire & Humber Patient Safety Translational Research Centre, where he studies the design and evaluation of digital innovation for patient safety.